Electronic clinical outcome assessment (eCOA) systems are used to collect data on patient outcomes in clinical trials. eCOA systems can capture data from patients, clinicians, and observers documenting a patient's condition, symptoms, and treatment effects.
Historically, it has not always been possible to action any patient-reported data changes in the eCOA software due to the lack of clarity around the process of reviewing and authorizing these changes, as well as lack of edit functionality for the data in the computerized systems being used.
This has created challenges for participants, site personnel, clinical research associates, service providers, and sponsors alike. Each stakeholder works to fulfill their own obligations within the responsibility of the protocol, GCP, and regulations, but roles and responsibilities have not been clear.
This article looks into the background here—from collection of data, to establishing the chain of command in terms of making electronic patient-reported outcome (ePRO) data changes—and introduces a recently published paper that outlines a comprehensive new best practice recommendation.

How is trial data collected?
Clinical trial data is captured using validated questionnaires to ensure the response options are standardized across all participants. From disease symptoms and treatment side effects, to functional outcomes, whether physical, social, emotional or cognitive, patient-reported data informs decision-making and ultimately influences healthcare policy and practice.
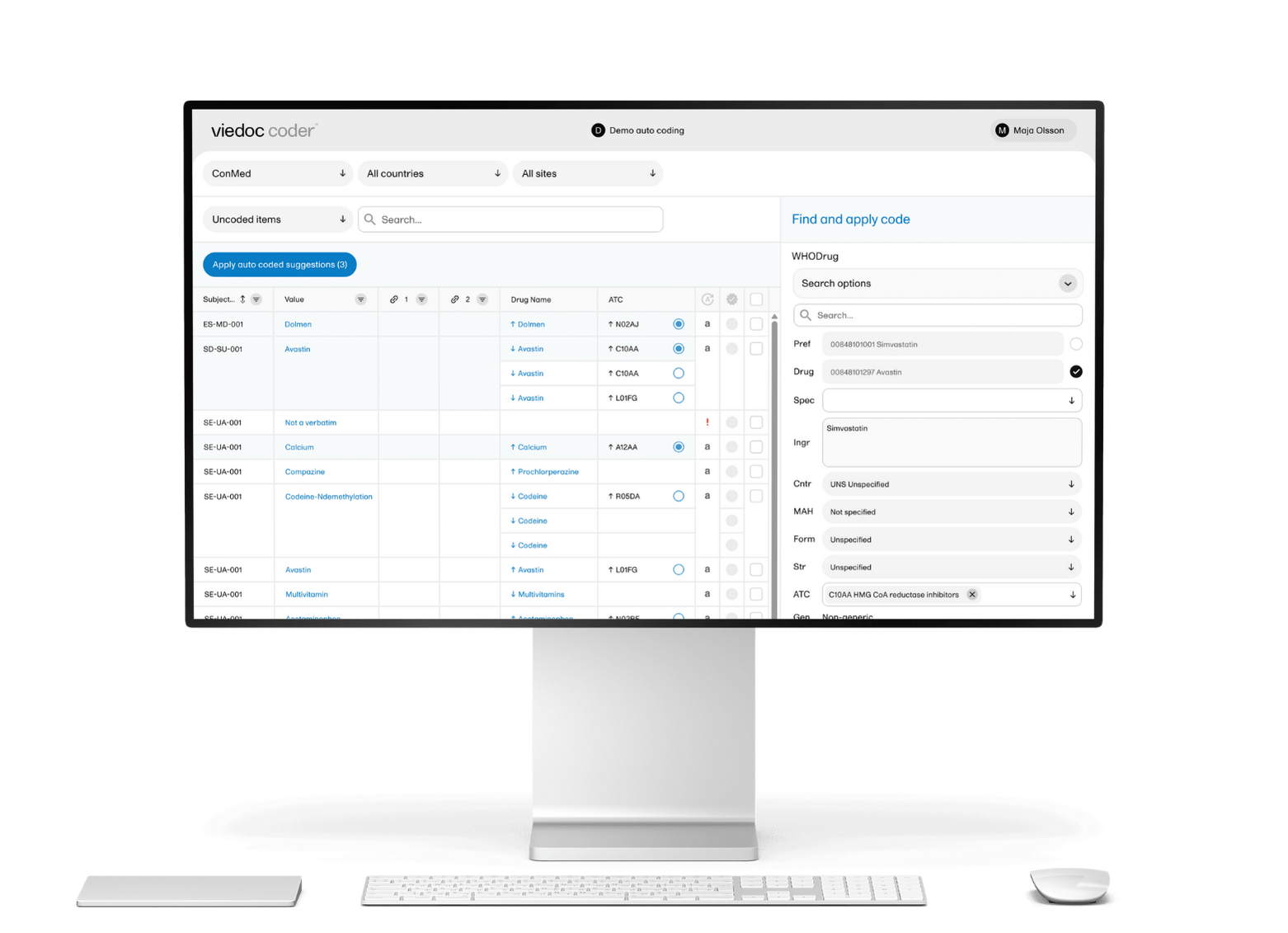
eCOA is a more accurate and efficient method of data collection than the traditional labor-intensive manual paper-based assessments. An ePRO/eCOA software such as Viedoc Me can directly capture trial data that’s been reported via a patient's smart device, improving data quality, and increasing patient compliance.

How have data changes been managed to date?
Current regulations divide responsibilities between site and sponsor, where the site should have control over the source records and maintenance of those records, and the sponsor should have oversight over the conduct of the trial in accordance with the protocol.
Regulatory requirements across the board state that, in order to maintain the integrity and accuracy of source records, any changes or corrections to data must be dated, initialed, and explained.
It is inevitable that mistakes will be made, but any proposed changes to ePRO software data need to be carefully managed, especially if they could be attributed to recall bias. For example, a patient changing a response the day after they recorded it because in hindsight they decided a symptom or side effect wasn’t as bad as they initially thought. This is a valid concern as pain memory is notoriously bad, so it’s important to push back on that type of change.
However if, say, a site coordinator enters data under the wrong subject and realizes their mistake shortly after, the data must be moved to the correct place as quickly as possible.
The industry has desperately needed a scalable process for submitting, evaluating, discussing, and implementing DCRs for some time. In fact, because of the lack of clear direction, most service providers have been agreeing with their sponsors not to allow any changes to patient-entered data. The regulatory authorities have indicated that this approach is not acceptable.

A new best practice recommendation
Viedoc’s Regulatory Affairs Manager, Alan Yeomans, was part of a team of specialists from the Critical Path Institute’s PRO Consortium, eCOA Consortium, and eClinical Forum, who recently got together to take an in-depth look at the process of performing and documenting changes to PRO data.
The resulting paper, Best Practice Recommendations for Electronic Clinical Outcome Assessment Data Changes, was published on SCDM’s website in December 2023. It offers a long overdue outline of trial-specific processes with agreed roles and responsibilities, and describes a workflow that allows investigators to maintain data accuracy, ensuring any data changes made are supported by clear justification and context.
Alan recalls “We started out thinking we’d just make a good process for changing data but quickly realized it wasn't that easy. We kept arguing back and forth and back and forth. So we defined the core principles, and then decided we needed an oversight plan, or data management plan, to regulate how to handle PRO data changes.”
Alan goes on to clarify “The site always has to have control. They are the ones who are responsible for the data. And the sponsor has to have their oversight. They have to be able to see what's happening in the study.”
“Data changes should not compromise compliance with ALCOA+, so you still have to follow all the same regulations for data changes as you do during the initial data collection. And all changes should be fully recorded with audit trails” confirms Alan.

What should an oversight plan include?
Having an oversight plan in place means there should be a clear workflow for any change request scenario. The plan should define procedural and technical details related to each type of change. It will also define which DCR types are critical (changes that require follow-up with the site, and notification/discussion with the sponsor/CRO, or both), and which are procedural (do not require follow-up).
A good start would be to categorize the protocol data into critical and procedural data points, and document these in the oversight plan. The plan should then outline the process for each type of data change in a way that is consistent with the protocol and maintains data integrity, and which also satisfies the regulations regarding site control over source records and sponsor oversight of the trial.

Viedoc supports eCOA data integrity
Viedoc Me is an ePRO/eCOA software that integrates with the Viedoc system and allows patients to enter data directly into the platform using their smartphones, tablets, or computers. This helps to improve the efficiency and accuracy of data collection, and can reduce the need for in-person visits.
It also encourages trial retention. The smoother a trial runs, the better the experience for the patient, and the more likely they will stick with the trial. And being able to use their own device to enter data gives them greater control, encouraging buy-in.
Below are some of the benefits of using Viedoc Me as your eCOA software:
Faster data collection
Collects data directly from the patient, eliminating the need for data entry and transcription errors.
Integrated solution
Allows users to set up forms that can be posted to patients or made part of the CRF.
File upload
Allows patients to submit image documentation directly from their smartphones.
Patient engagement
User-friendly interface helps to enhance patient engagement and compliance.
Real-time data capture
Facilitates real-time data capture, improving the quality and timeliness of clinical trial data.


/new-year.jpg)
/female-doctor-with-tablet.jpg)